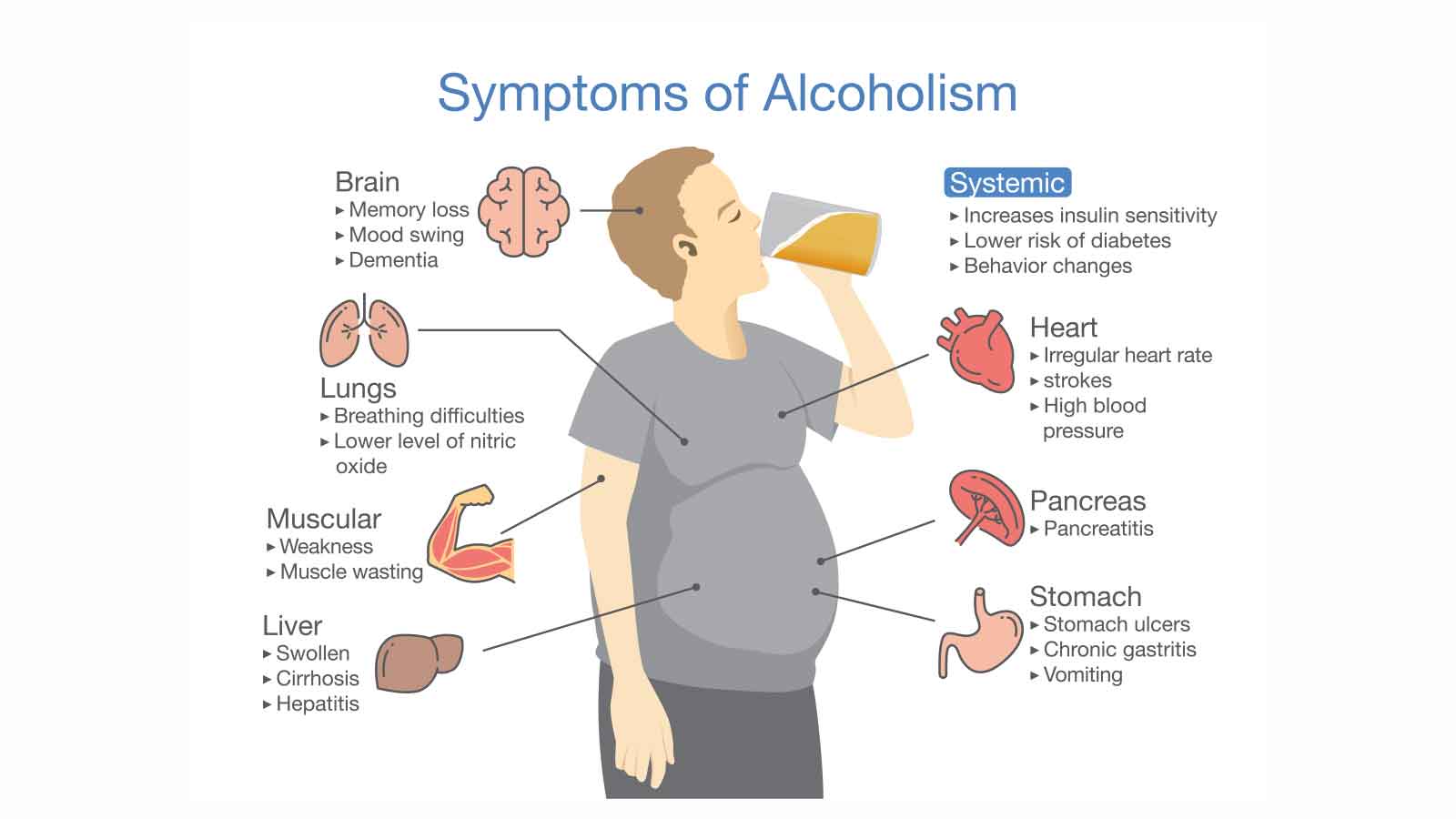
Most people are aware of the well-known dangers of alcohol misuse, such as liver disease, cardiovascular issues, or even accidents and injuries born out of misadventure and poor judgment. The consequences of drinking alcohol frequently and above the recommended weekly units are widely reported, also including an increased risk of cancers, mental health disorders, nutritional deficiencies, and reduced immune function.
But most people are unaware of the sheer number of illnesses and disorders that are a direct result of too much alcohol consumption, which are officially in excess of 200 known conditions. That's quite a staggering number when you think about it, made even more alarming when considering the number of people who succumb to alcohol-related illness each year.
In fact, 5-10% of adults worldwide experience some form of significant alcohol-related health issues at some point during their lives.
However, there is one illness in particular that deserves more recognition, both for its seriousness and prevalence. An illness which, if serious enough, is quite a terrifying prospect for both sufferers and loved ones: the condition known as alcohol-related brain impairment - also known as alcohol-related brain damage and alcoholic dementia, among others.
Commonly Overlooked
While much of the general discourse centers on afflictions like liver disease and alcohol overdose, the harmful impact of alcohol-related brain damage is surprisingly under-discussed (outside of the medical and health profession) even though it is alarmingly common.
Contrary to popular belief, alcoholic brain damage (or 'wet brain', to use the more colloquial term) isn't exclusive to long-term heavy drinkers. Even those who drink alcohol moderately can experience permanent brain damage.
Through this article, we shall explore the causes, treatment options, and general overview of the condition sometimes referred to as Wernicke Korsakoff Syndrome.
What Exactly is ARBD, and Who Is at Risk?
Alcohol-related brain damage, frequently abbreviated as ARBD, is a serious brain disorder, directly correlated with prolonged alcohol consumption habits. However, this isn't just about the occasional leisurely drink; it is a result of consistent alcohol misuse over the years, frequently distinguished by heavy drinking or binge drinking episodes.
While alcohol misuse is a definite concern across all age groups, research suggests that those most susceptible to the negative effects and symptoms of ARBD are people aged between 40 and 50.
A commonly misunderstood element of Wernicke Korsakoff syndrome or alcohol-related dementia is that the damage isn't limited exclusively to the quantity of alcohol consumed - but more the regularity of heavy consumption patterns.
Anyone who may drink heavily on a frequent basis is of potentially quite extreme risk - but even if a person drinks only a few units per day - but does so most days - they could also be exposed to the condition.
As alcohol use disorder continues to grow, understanding who is at risk is an important factor in reducing the number of sufferers. This particularly nasty brain disorder reminds us that drinking alcohol irresponsibly has far-lasting implications and that frequent alcohol abuse targets all genders and age groups.
The Long-Term Consequences of Excessive Alcohol Consumption
Consistent excessive alcohol consumption, especially when it exceeds the recommended alcohol limits, can have quite dire consequences, especially on the brain's ability to function properly.
Although, it is worth pointing out once again that this isn't about the occasional overindulgence or infrequent binge drinking; it is more the sustained, heavy drinking that contributes to significant brain impairment over the years.
This damage manifests as alcohol-related brain damage (ARBD) or alcohol-related brain injury (ARBI), with symptoms that vary in intensity. For some, the effects may be almost quite subtle at first, presenting as mild cognitive impairment (MCI). Occasional memory lapses or a slight struggle in clear thinking might seem harmless. However, even this mild symptom comes with a risk: if the person continues their patterns of alcohol misuse, they risk increasing their brain damage.
For other more unfortunate people, the consequences are far more severe, where disorders categorized as alcohol-induced dementia or Wernicke-Korsakoff syndrome become evident. People with these conditions often struggle with basic day-to-day tasks, similar in many ways to the challenges faced by those living with severe brain injuries like Alzheimer’s disease.
The correlation between heavy drinking and such awfully debilitating conditions as Wernicke Korsakoff Syndrome demonstrates the brain's vulnerability to sustained alcohol abuse, which is similar in many ways to the consequences of heavy, long-term substance abuse.
ARBD vs. Dementia: What's the Difference?
While both alcohol-related brain damage and conditions like Alzheimer's fall under the broad category of cognitive disorders, they share unique characteristics and progression patterns over time. Notably, however, ARBD offers some glimmer of hope not available to people suffering from many dementia types, such as Alzheimer’s disease. With Alzheimer's, there's an inevitable worsening of the disease over time.
However, ARBD does have the potential for reversibility to various degrees. This means that if a person with alcohol-related brain damage stops their alcohol consumption and receives the right levels of support, there is a very real possibility for improvement.
With the right measures in place, including abstaining from alcohol, adopting a healthy diet, and making the most of support groups, these people can experience significant restoration in their cognitive functions. While a full recovery is not always likely, they might reclaim their lost memory, refine their thinking skills, and enhance their overall ability to function independently.
The brain is mercifully resilient in many cases - providing intervention and cessation of alcohol misuse is adhered to - potentially reversing the negative effects of ARBD.
What Constitutes Excessive Drinking?
When consumed in moderation, alcohol is a normal part of social rituals or relaxation methods for some people. However, understanding when how much alcohol is too much is something everyone should be aware of, given the potential negative effects on a person's brain and overall health.
To gauge this, health professionals often use a measure known as a 'unit' of alcohol. By checking the label on alcoholic beverages before a person drinks, one can determine the number of units contained within. A bottle of beer, for example, might contain somewhere in the region of two units.
Most health authorities suggest an upper limit of around 15 units of alcohol per week, advocating for this to be dispersed over three days or more and certainly not 'all in one session'. The reason behind this recommendation lies in the harm that binge drinking can inflict on the brain and nervous system.
When someone's alcohol consumption exceeds approximately 25 units weekly, it might begin to hamper their overall brain function and impede their ability to perform tasks efficiently and effectively.
But what exactly is 'binge drinking'? The term speaks for itself to some degree, referring to the practice of consuming a significant volume of alcohol in a very short interval, such as over a couple of hours or one single evening. For the purpose of clarity, this would be similar to males ingesting eight or more units and women taking in six or more.
Click here for a detailed breakdown of how long alcohol stays in your system
Given the vulnerability of the brain in senior citizens and overall health to the repercussions of alcohol misuse, it is suggested that the elderly should adhere to even stricter limits. After all, their susceptibility to alcohol's effects, from mood changes to more severe brain impairment, is far greater than a person in their twenties.
The Primary Causes of Alcohol-Related Brain Damage
But what is it, exactly, that causes such awful devastation to the brain? The potential repercussions of excessive alcohol consumption are varied, impacting the brain's ability to function optimally, but how does brain damage from alcohol manifest on a biological level?
To understand those reasons, we need to take a look at the science behind alcohol and brain damage.
Nerve Cells' Degeneration
Heavy drinking, particularly when over the recommended limits, has a toxic effect on nerve cells. Over prolonged periods, too much alcohol can trigger the death of brain cells, resulting in a reduction in brain tissue. With a diminishing count of brain cells, the transmission of essential messages across the brain becomes hindered.
Vascular Damage
Beyond its direct impact on brain cells, alcohol misuse can wreak havoc on the blood vessels within the brain. Coupled with the escalation in blood pressure that often accompanies chronic drinking, this presents an increased risk of strokes. This happens because a stroke event signifies a deprivation of oxygen to the brain, leading to potential brain damage.
Thiamine (Vitamin B1) Deficiency
With many alcohol-induced brain injuries, there is a severe deficiency in thiamine. Alcohol impedes the body's ability to absorb and utilize this critical vitamin, which is important for the brain's ability to function properly. People battling alcohol use disorder often have poor nutrition, drawing much of their caloric intake from alcoholic beverages, commonly leading to thiamine deficiency.
These patterns, over extended periods and combined with generally poor health, put these people at an increased risk of malnutrition, further increasing the chances of thiamine deficiency.
Greater Susceptibility to Severe Brain Injury
People who drink heavily are invariably more prone to repetitive head injuries. The influence of alcohol can result in falls, accidental collisions, or becoming targets of violent acts, all of which can culminate in trauma to the brain.
Head injury may sound like a far-reaching consequence of too much alcohol, but make no mistake about it - the chances of a person suffering head injuries, while relatively remote, may happen more often than you might imagine.
In people diagnosed with ARBD, it's not uncommon to identify a combination of all of these damages. Although specific forms of ARBD, like Wernicke-Korsakoff syndrome, bear a direct correlation with particular causes, such as thiamine deficiency in this case.
Are There Different Types of ARBD?
Usually, a person is diagnosed with a specific type of ARBD by a medical or health professional. Depending on their symptoms, they may have one of several conditions, including the following:
- Alcohol-related ‘dementia’
- Wernicke–Korsakoff syndrome (also called amnestic syndrome)
- Traumatic brain injury
- Alcohol-related stroke
- Other rarer forms of ARBD
- Fetal Alcohol Syndrome (in pregnancy)
The two main types of ARBD that can cause symptoms of dementia are alcohol-related ‘dementia’ and Wernicke–Korsakoff syndrome. While neither of these are actual types of dementia (remember, you cannot get better from dementia) there is a reasonable chance of recovery in both of these conditions.
Alcohol Brain Damage Symptoms
Chronic misuse of alcohol can lead to various neurological and cognitive issues, with symptoms presenting in various physical and mental ways. Some of the more prominent signs of alcoholism include:
- Cognitive decline
- Mental confusion
- Memory problems
- Poor balance
- Abnormal eye movements
- Blurred vision
- Clammy skin
- Muscle coordination issues
- Erratic behavior
- Poor decision-making & life choices
- Hepatic encephalopathy
Treatment for Alcohol Related Brain Impairment

The simple fact of the matter is that prolonged misuse of alcohol contributes to a higher risk of neurological disorders like ARBD. Recovery, as with many other additions, starts with the personal realization of this issue: the sufferer must acknowledge that they misuse alcohol. Only then can the withdrawal process start.
The premise of halting alcohol might seem simple enough, but alcohol withdrawal symptoms can be quite brutal, with symptoms like seizures and hallucinations a real possibility if not monitored by qualified professionals. Miracles Asia provides resources and expert support to ensure this withdrawal process is safer, more efficient, and with a greater chance of long-term success.
With personalized treatment that includes customized detox plans & therapy sessions, and prescribed medications, our luxury rehab center, located on the beautiful island of Phuket, Thailand, offers clients a truly holistic and tailored approach to guide you or your loved one toward a healthier, alcohol-free future.
At Miracles Asia, you'll find counseling, medical support, and the means to embrace sobriety without fear. If you or a loved one is struggling with an addiction or self-destructive habit, don't hesitate to reach out to our Admissions Team for a free assessment call that can get you or your loved one the help they deserve.